Showing posts from category gender.
-
Perfect Storm? Population Pressures, Natural Resource Constraints, and Climate Change in Bangladesh
›Few nations are more at risk from climate change’s destructive effects than Bangladesh, a low-lying, lower-riparian, populous, impoverished, and natural disaster-prone nation. The UN Intergovernmental Panel on Climate Change estimates that by 2050, sea levels in Bangladesh will have risen by two to three feet, obliterating a fifth of the country’s landmass and displacing at least 20 million people. On September 19, the Wilson Center’s Asia Program, with assistance from ECSP and the Comparative Urban Studies Project, hosted a conference that examined Bangladesh’s imperiled environmental security.
Climate Change and Population
The first panel focused on manifestations, drivers, and risks. Ali Riaz addressed the threat of climate refugees. Environmental stress, he said, may produce two possible responses: fight (civil conflict or external aggression) or flight (migration). In Bangladesh, the latter is the more likely outcome. Coastal communities, overwhelmed by rising sea levels and flooding, could migrate to Bangladesh’s urban areas or into neighboring India. Both scenarios pose challenges for the state, which already struggles to provide services to its urban masses and has shaky relations with New Delhi.
Mohamed Khalequzzaman examined Bangladesh’s geological vulnerability in the context of climate change. In a deltaic nation like Bangladesh, he explained, sedimentation levels must keep up with rates of sea level rise to prevent the nation from drowning. However, sediment levels now fall below 5 millimeters (mm) per year – short of the 6.5 mm Khalequzzaman calculates are necessary to keep pace with projected sea level rises. He lamented the nation’s tendency to construct large dams and embankments in the Bengal Delta, which “isolate coastal ecosystems from natural sedimentation,” he said, and result in lower land elevations relative to rising sea levels.
Adnan Morshed declared that Bangladesh’s geographic center – not its southern, flood-prone coastal regions – constitutes the nation’s chief climate change threat. Here, Dhaka’s urbanization is “destroying” Bangladesh’s environment, he said. Impelled by immense population growth (2,200 people enter Dhaka each day) and the need for land, people are occupying “vital wetlands” and rivers on the city’s eastern and western peripheries. “Manhattan-style” urban grid patterns now dominate wetlands and several rivers have become converted into land. Exacerbating this urbanization-driven environmental stress are highly polluting wetlands-based brickfields (necessary to satisfy Dhaka’s construction needs) and city vehicular gas emissions.
Adaptation Responses
The second panel considered possible responses to Bangladesh’s environmental security challenges. Roger-Mark De Souza trumpeted the imperative of more gender-inclusive policies. Environmental insecurity affects women and girls disproportionately, he said. When Bangladesh is stricken by floods, females must work harder to secure drinking water and to tend to the ill; they must often take off from school; and they face a heightened risk of sexual exploitation – due, in great part, to the lack of separate facilities for women in cyclone shelters. He reported that such conditions have often led to early forced marriages after cyclones.
Shamarukh Mohiuddin discussed possible U.S. responses. On the whole, American funding for global climate change adaptation programs has lagged and initiatives that are funded often focus more on short-term mitigation (such as emissions reductions) rather than adaptation. She recommended that Washington’s Bangladesh-based adaptation efforts be better coordinated with those of other donors.
Mohiuddin also suggested that to convey a greater sense of urgency, Bangladesh’s climate change threats should be more explicitly linked to national security – and particularly to how America’s strategic ally, India, would be affected by climate refugees fleeing Bangladesh.Philip J. DeCosse highlighted Bangladeshi government success stories in the famed Sundarbans – one of the world’s largest mangrove forests. Officials have banned commercial harvesting in some areas of the forests and shut down a highly polluting paper mill. He also praised civil society and the media for bringing attention to the Sundarban’s environmental vulnerability. As a result of efforts such as these, the Sundarbans are “coming back,” he said, with mangrove species growing anew. Thanks to a range of actors – from the forestry department to civil society – these forests are also now being “governed more than managed,” said DeCosse.
The Sundarbans – click to view larger map.
DeCosse’s fellow panelists identified additional hopeful signs. Morshed shared a photograph of a green, pristine park in Dhaka. De Souza underscored how family planning programs have worked in Bangladesh in the past, with fertility rates declining considerably in recent years, and several speakers spotlighted efforts by civil society and the media to bring greater attention to Bangladesh’s environmental security imperatives.
Nonetheless, major challenges remain, and panelists offered a panoply of recommendations. Khalequzzaman called for a major geological study of soil loss and siltation. De Souza implored Bangladesh to ensure that women’s roles and family planning considerations are featured in climate change negotiations and adaptation policies. Morshed advocated for imposing urban growth boundaries and enhancing public transport in cities. And several speakers spoke of the need to pursue more effective natural-resource-sharing arrangements with India. Ultimately, in the words of De Souza, it may not be possible to eliminate Bangladesh’s “perfect storm” – but much can be done to calm it.
Event ResourcesMichael Kugelman is a program associate with the Wilson Center’s Asia Program.
Sources: UN.
Photo/Image Credit: “Precarious Living, Dhaka,” courtesy of flickr user Michael Foley Photography; “Impact of Sea Level Rise in Bangladesh,” courtesy of UNEP; and the Sundarbans courtesy of Google Maps. -
John Donnelly, Global Post
Family Planning and Seven Billion at the Aspen Institute
›September 9, 2011 // By Wilson Center Staff
The original version of this article, by John Donnelly, appeared on Global Post.
Sometime this fall, the world’s population will reach 7 billion people. Experts now forecast that by 2050, the population could be 10 billion.
Those numbers, said the former presidents of Chile and Latvia at an event in Washington D.C., Wednesday night, should force policy makers to focus more intently on making family planning much more widely available in the developing world.
“When we are 9, 10 billion people, what are we going to do? Go to Mars? Go to the moon?” said Michelle Bachelet, the former president of Chile and now the Under Secretary-General and Executive Director of UN Women, the latest agency created by the United Nations. “We are really going to have huge problems. Family planning is a huge issue.”
Her comments came during a series of discussions organized by Aspen Global Health and Development called “7 Billion: Conversations that Matter.” The talks, funded in part by the U.S. Agency for International Development, have often centered on global health issues, and Wednesday’s event was no different.
Continue reading on Global Post.
Video Credit: The Aspen Institute. -
The Role of Faith-Based Organizations in Maternal and Newborn Health Care
›Government and nongovernmental organizations have consistently played a key role in addressing maternal mortality. While these initiatives are well documented, the role of faith-based organizations (FBOs) in maternal and newborn health is less well understood.
In November, the Wilson Center’s Advancing Policy Dialogue to Improve Maternal Health series will bring diverse institutions together such as the Pakistan Initiative for Mothers and Newborns (PAIMAN) and Pathfinder International to discuss country experiences and evaluate opportunities for overcoming challenges.
According to the World Health Organization, FBOs own up to 70 percent of the health infrastructure in sub-Saharan African countries and often work in remote regions where government and NGO services are limited. FBO’s are critical to improving maternal health as they fill gaps in the health system – particularly in low-resource settings – and approaching culturally sensitive barriers that often prevent mothers from seeking health care.
The level of trust communities place on their religious leaders explains one of the main reasons why FBOs are attaining success. A study conducted by Pew Charitable Trust found that a vast majority of people in sub-Saharan Africa identify themselves as adherents of Christianity or Islam, and approximately 75 percent trust their religious leaders.
As partnerships with FBO’s increase, it is imperative that organizations share their lessons learned and identify capacity and knowledge gaps in order to improve effectiveness.
Pakistan Initiative for Mothers and Newborns
The Pakistan Initiative for Mothers and Newborns (PAIMAN), which started out as a six-year project funded by USAID and led by JSI Research and Training Institute, is a strong example of a program incorporating faith to improve maternal mortality rates. The project aims to ensure that women have access to skilled birth attendants during and immediately after giving birth. Additionally, the project focused on increasing the quality of care both in the public and health sectors. PAIMAN was able to achieve substantial success by utilizing various communication interventions such as mass media, community media, and advocacy efforts. One of the most successful initiatives PAIMAN organized was reaching out to 1,000 religious scholars, known as ulamas, to deliver frequent messages on maternal and newborn health care. Since its initiation, this project has “saved more than 30,000 newborn lives resulting in a 23 percent decrease in neonatal mortality,” according to their numbers.
Pathfinder International
Pathfinder International is another great example of an organization that has understood the value of FBOs and worked in collaboration with them to achieve results for maternal health. Pathfinder has worked in numerous countries including Nigeria, Ghana, Ethiopia, Egypt, Uganda, Kenya, and Bangladesh to educate religious leaders and communities on communication strategies for improving maternal health behaviors.
In Ethiopia, Pathfinder organized over 250 religious leaders representing the Orthodox Christian, Catholic, Protestant, Seventh Day Adventist, Mekaneyesus Christian, and Muslim faiths to educate them about maternal mortality. At the conclusion of the seminar, the religious leaders agreed to condemn a host of harmful traditional practices, including female genital cutting, marriage by abduction, early marriage, rape, and unsafe abortion and agreed that they are not required by the Bible or Korean. Religious leaders in Egypt also came to similar conclusions after participating in these types of seminars.
“By helping religious leaders see the links between reproductive health and families’ well-being, Pathfinder enables them to become committed advocates for positive reform,” wrote Mary K. Burke, technical communications associate at Pathfinder International in the 2006 report, Advancing Reproductive Health and Family Planning through Religious Leaders.
Challenges: Equipping and Encouraging
Despite the prevalence of success stories among FBOs to improve maternal mortality, challenges do exist. For instance, although religious leaders are highly respected by their communities, their teachings become useless, as pointed out by a USAID-sponsored Extending Service Delivery Project report, unless they are also properly trained and equipped with the latest service delivery systems and scientific information.
The report also describes the importance of cooperation and support from the government and decision-making representatives. If the private, public, and government sectors are fragmented and no formal recognition exists to acknowledge the work of religious leaders for improving maternal mortality, then success may be significantly hampered.
To learn more about the role of faith-based organizations in women’s health, be sure to check out the Global Health Initiative event on FBOs coming in November, with representatives from PAIMAN, Pathfinder International, and others.
Sources: Extending Service Delivery Project, JSI Research and Training Institute, Pathfinder International, Pew Charitable Trust, USAID, World Health Organization.
Photo Credit: “Woolly hats needed,” courtesy of flickr user Church Mission Society (CMS). -
Laurie Mazur, RH Reality Check
Why Women’s Rights Are Key to Thriving in the Age of the “Black Swan”
›August 16, 2011 // By Wilson Center StaffThe original version of this article, by Laurie Mazur, appeared on the RH Reality Check blog.
Welcome to the age of the “black swan.”
The tornado that nearly leveled the city of Joplin, Missouri in May was a black swan; so was the 9.0 magnitude earthquake and tsunami that rocked Japan in March; and the “hundred-year floods” that now take place every couple of years in the American Midwest.
A black swan is a low-probability, high-impact event that tears at the very fabric of civilization. And they are becoming more common: Weather-related disasters spiked in 2010, killing nearly 300,000 people and costing $130 billion.
Black swan events are proliferating for many reasons – notably climate change and the growing scale and interconnectedness of the human enterprise. World population doubled in the last half-century to just under seven billion people, so there are simply more people living in harm’s way, on geologic faults and along vulnerable coastlines. As the human enterprise has grown, we have reshaped natural systems to meet human needs, weakening resilience of ecosystems, and by extension our own. In effect, we have re-engineered the planet and ushered in a new era of radical instability.
At the same time, the world’s people are increasingly linked by systems of staggering complexity and size: think of electrical grids and financial markets. What were once local disasters now reverberate across the globe.
So what does this have to do with women’s rights, you may ask? A lot, as it turns out. The great challenge of the 21st century is to build societies that can cope with the flock of black swans that are headed our way. Advancing and securing women’s rights, especially reproductive rights, is central to meeting that challenge.
Continue reading on RH Reality Check.
Laurie Mazur is the editor of A Pivotal Moment: Population, Justice & the Environmental Challenge, which received a Global Media Award from the Population Institute in 2010.
Sources: Munich Re.
Photo Credut: “Cygnus atratus (Black Swan),” courtesy flickr user Arthur Chapman. -
Conflict Minerals in the DRC: Still Fighting Over the Dodd-Frank Act, One Year Later
›August 11, 2011 // By Schuyler Null
One year after the Dodd-Frank Act passed Congress with a provision that was aimed at preventing the sourcing of “conflict minerals” by SEC-registered companies, backlash seems to be growing over the impact of the measure, particularly on artisanal miners in the Democratic Republic of the Congo (DRC).
-
Fistula, Stigmatization, and Development
›Although obstetric fistula may not be as widely recognized as other maternal health issues, the Fistula Foundation estimates that over two million women and girls in developing countries suffer from this condition today. The World Health Organization has labeled it as “the single most dramatic aftermath of neglected childbirth.”
Obstetric fistula is a devastating condition often resulting from obstructed labor that can cause infections, incontinence, and even paralysis. The condition largely afflicts poor, rural, and illiterate women in developing countries who lack resources and access to emergency care and surgery, and sufferers often face an additional burden of social stigma.
Economic Development and Social Standing
Poor infrastructure and poverty significantly increases the occurrence rate of obstetric fistula. Lewis Wall, in an article for The Lancet, writes that “poverty is the breeding-ground where obstetric fistulas thrive.” Wall cites early marriage, low social status of women, malnutrition, inadequately developed social and economic infrastructures, and lack of access to emergency obstetric services as being major contributors of fistulas in developing countries.
Additionally, “postponing the age of marriage and delaying childbirth can significantly reduce the risk of subjecting young women to the arduous labor that induces fistulas,” wrote Sonny Inbaraj of Inter Press Service News Agency (IPS) in an article about how fistula makes social outcasts of child brides.
In most developing societies where child marriage is common, the social standing of women is defined largely in terms of marriage and childbearing. Child marriages are typically arranged without the knowledge or consent of the girls involved. The norms emphasize a girl’s domestic roles and de-emphasize investments such as education.
Stigmatization of Fistula
There is an undeniable link between fistula and social stigmatization. Rather than receiving assistance from their families and communities, women are often ostracized and in many instances exiled from their communities. This is especially true in developing countries where “the role of women is merely limited to providing sexual satisfaction for their husbands, [and] producing children,” said Dr. Catherine Hamlin, founder of the Addis Ababa Fistula Hospital, in an interview with IPS.
“Many women and girls with fistula endure lives of shame, misery, violence, and poverty,” said Agnes Odhiambo, Africa women’s rights researcher and author of ‘I Am Not Dead, But I Am Not Living‘: Barriers to Fistula Prevention and Treatment in Kenya, in a Human Rights Watch article. Human Rights Watch has focused on fistula, recognizing that birth is a human rights issue. Ignoring the issues of women and girls only diminishes progress on human rights and sends a message that says the rights of women do not deserve adequate attention.
Prevention Efforts
Thus far the fight to end fistula has attracted various government agencies and organizations including USAID, UNFPA, EngenderHealth, Maternal Health Task Force, and the Human Rights Watch. Outstanding individuals have also played a key role in fistula prevention efforts, like Drs. Reginald and Catherine Hamlin, Australian gynecologists who came to Addis Ababa in 1959 for temporary medical work, but after hearing heart-breaking stories from fistula patients, they decided to move to Ethiopia permanently and open the Addis Ababa Fistula Hospital. As the only hospital dedicated exclusively to women with obstetric fistula, the hospital provides care free of change, and has done so since 1974.
Although fistula has gotten some support and attention, the need to scale-up the prevention initiatives has never been greater. As a result of the “poverty and the stigma associated with their condition, most women living with fistulas remain invisible to policy makers both in their own countries and abroad,” wrote Inbaraj on IPS.
“Preventing fistula and restoring women’s health and dignity requires more than good policies on paper,” said Odhiambo at Human Rights Watch. Seriously tackling the issue will require much more than traditional medical and public health interventions – prevention efforts must also take into account underlying social issues, food and economic security.
Sources: The Addis Ababa Fistula Hospital, Campaign to End Fistula, The Center for Global Development, The Fistula Foundation, Human Rights Watch, The Lancet, World Health Organization.
Photo Credit: “Hauwa’u, 25, mother from Rogogo community,” courtesy of flicker user DFID-UK Department for International Development. -
Sajeda Amin on Population Growth, Urbanization, and Gender Rights in Bangladesh
› “One of the reasons why population grows very rapidly in Bangladesh is women get married very early and have children very early,” the Population Council’s Sajeda Amin told ECSP in a recent interview. “So even though they are only having two children, they are having them at an average age of around 20. As demographers would say, women ‘replace’ themselves very rapidly.”
“One of the reasons why population grows very rapidly in Bangladesh is women get married very early and have children very early,” the Population Council’s Sajeda Amin told ECSP in a recent interview. “So even though they are only having two children, they are having them at an average age of around 20. As demographers would say, women ‘replace’ themselves very rapidly.”
Largely through the promotion of contraceptive use, family planning programs implemented over the past 35 years by the Bangladeshi government and a variety of NGOs have helped lower the country’s total fertility rate to 2.7 from 6.5 in the mid-1970s. To build on this progress, the Population Council has joined a consortium of other organizations – including the Bangladesh Legal Aid and Services Trust, Marie Stopes International, and We Can End All Violence Against Women – to launch the Growing Up Safe and Healthy (SAFE) project in Amin’s native Dhaka and other Bangladeshi cities.
Currently nearing the completion of its first year, the four-year initiative has several aims, among them increasing access to reproductive healthcare services for adolescent girls and young women and bolstering social services to protect those populations from (and offer treatment for) gender-based violence. The project also looks to strengthen laws designed to reduce the prevalence of child marriage – a long-standing Bangladeshi institution that keeps population growth rates high while denying many young women the opportunity to pursue economic and educational advancement.
A Focus on Gender and Climate
Amin says the SAFE project boasts several qualities that collectively set the initiative apart from similar-minded programs in Bangladesh dealing with gender and poverty. These include a strong research component incorporating quantitative and qualitative analysis; the holistic nature of the program, which incorporates educational outreach, livelihood development, and legal empowerment; a commitment to working with both male and female populations; and an emphasis on interventions targeting young people, with the hope that such efforts will allow adolescents to make better-informed decisions about future relationships and reproductive health, thus reducing the likelihood of gender-based violence.
Finally, while many existing gender-based programs focus exclusively on rural communities, Amin points out that the SAFE project also stands apart because of its focus on the country’s rapidly expanding urban areas. To date, the initiative is focusing many of its early interventions in a Dhaka slum that has seen an influx of rural migrants in recent years due to climate-change impacts in the country’s low-lying coastal areas.
“A lot of the big problems in Bangladesh now are climate-driven in the sense of creating mass movements out of areas that are particularly vulnerable or have been hit by a major storm,” Amin said. “Usually these are people who, once they lose their homes and their livelihoods, will have no choice but to move to urban areas, and that’s a process that is kind of a big outstanding issue in Bangladesh now.”
By building programming around girls and young women in such communities, the SAFE project is looking to spark change from the bottom up, prioritizing the unmet health and social needs of some of Bangladesh’s most vulnerable populations.
The “Pop Audio” series is also available as podcasts on iTunes.
Sources: Global Post, Ministry of Health and Family Welfare (Bangladesh), Shaikh and Becker (1985). -
Reducing Health Inequities to Better Weather Climate Change
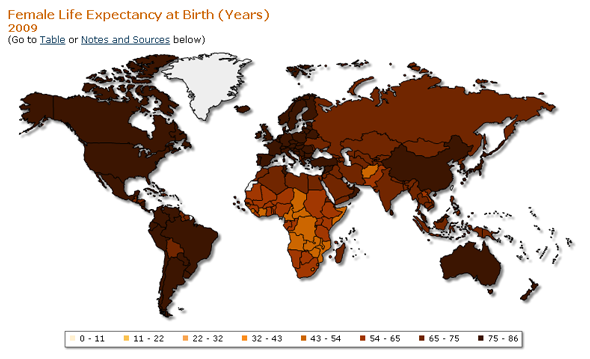
›In an article appearing in the summer issue of Global Health, Dr. Margaret Chan, director-general of the World Health Organization (WHO), brings to light what she calls the starkest statistic in public health: the vast difference in the mortality rates between rich and poor countries. For example, the life expectancy of a girl is doubled if she is born in a developed country rather than in a developing country. Chan writes that efforts to improve health in developing countries now face an additional obstacle: “a climate that has begun to change.”
Climate change’s effect on health has increasingly moved into the spotlight over the past year: DARA’s Climate Vulnerability Monitor measures the toll that climate change took in 2010 on human health, estimating some 350,000 people died last year from diseases related to climate change. The majority of these deaths took place in sub-Saharan Africa, where weak health systems already struggle to deal with the disproportionate disease burden found in the region. The loss of “healthy life years” as a result of global environmental change is predicted to be 500 times greater in poor African populations than in European populations, according to The Lancet.
The majority of these deaths are due to climate change exacerbating already-prominent diseases and conditions, including malaria, diarrhea, and malnutrition. Environmental changes affect disease patterns and people’s access to food, water, sanitation, and shelter. The DARA Climate Vulnerability Monitor predicts that these effects will cause the number of deaths related to climate change to rise to 840,000 per year by 2030.
But few of these will be in developed countries. With strong health systems in place, they are not likely to feel the toll of a changing environment on their health. Reducing these inequities can only be achieved by alleviating poverty, which increases the capacity of individuals, their countries, and entire regions to adapt to climate change. It would be in all of our interests to do just this, writes Chan: “A world that is greatly out of balance is neither stable nor secure.”
Sarah Lindsay is a program assistant at the Ministerial Leadership Initiative for Global Health and a Masters candidate at American University.
Sources: DARA, Global Health, The Lancet, World Health Organization.
Image Credit: Henry J. Kaiser Family Foundation and the World Health Organization.